The term glaucoma is used to describe a group of eye diseases. In addition to damaging the eye’s optic nerve, glaucoma can result in vision loss and even blindness. About 3 million Americans have glaucoma, but the disease affects more than 67 million people worldwide and is the second leading cause of blindness. Glaucoma occurs in about 1% of the population above 50 years of age. The most frequent glaucoma diagnosis is primary open angle glaucoma (POAG). While there are no warning signs or obvious symptoms in the early stages of POAG, as the disease progresses, blind spots develop in peripheral (side) vision. Without testing, by the time that symptoms appear, vision damage is quite severe. Unlike POAG, patients with angle-closure glaucoma can experience attacks that include:
- severe pain in the eye or forehead
- redness of the eye
- decreased or blurred vision
- headache
- nausea
In either case, early detection can reduce the severity and impact of the disease. Several different sensing techniques are used to detect and measure the extent of glaucoma.
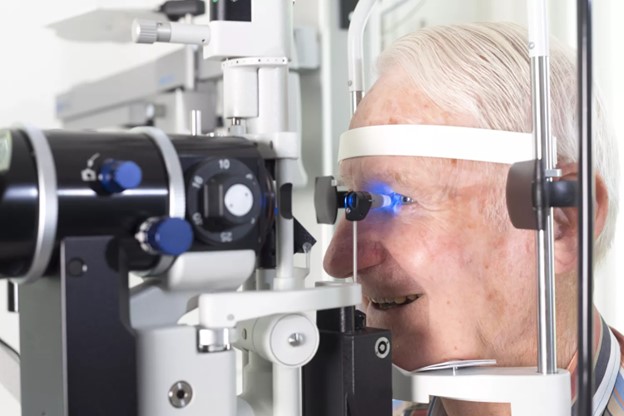
Tonometry is the noninvasive measurement of intraocular pressure (IOP). The normal eye pressure range for 90% of the population is between 10 and 21 millimeters of mercury (mmHg). Pressure measurements exceeding 20 mmHg are strong indicators of glaucoma. Unlike blood pressure or respiratory pressure measurements that are commonly made with microelectromechanical systems (MEMS) pressure sensors, eye pressure measurements require indirect sensing approaches.
Applanation tonometry, based on the Imbert-Fick principle, is the most widely used method. This principle states that the pressure inside an ideal dry, infinitely thin-walled sphere equals the force necessary to flatten its surface divided by the area of the flattening. The equation is the familiar definition of pressure:
P = F/A
where P = pressure, F = force, and A = area.
In applanation tonometry, the cornea is flattened (applanated), and the IOP is calculated by measuring the applanating force and the area flattened. Two popular methods that implement this technique include the Goldmann applanation tonometer and air-puff tonometry.
A Goldmann applanation tonometer measures the force necessary to flatten an area of the cornea with a fixed diameter of 3.06 mm. At this diameter, the capillary attraction of the tear film meniscus to the tonometer head counterbalances the material resistance of the cornea to flattening. The IOP (in mmHg) equals the applanating force (in gram-force) multiplied by 10.
Air-puff tonometry is a non-contact applanation method that uses a standardized puff of air to flatten the cornea. The system consists of a central air plenum to generate the puff of air with a light emitter and a light detector on opposite sides. When the pressure of the air pulse increases sufficiently to deform the cornea, the corneal surface responds like a plane mirror and reflects light to the detector. After recording the force of air required to flatten the cornea, the instrument displays the IOP that corresponds to that force.
An eye exam that only checks intraocular pressure is not enough to find glaucoma. Additional testing should include:
- inspecting the eyes’ drainage angle
- examining optic nerves for damage
- testing peripheral (side) vision
- taking a picture or making computer measurements of the optic nerves
- measuring the thickness of the corneas
References
Don’t Let Glaucoma Steal Your Sight!
What’s a Normal Eye Pressure Range?
Chapter 2: Intraocular Pressure and Aqueous Humor Dynamics
Image source: Westend61 / Getty Images How Tonometry Eye Pressure Tests Work
What Is Glaucoma? Symptoms, Causes, Diagnosis, Treatment
Featured image source: The best tonometer for home use to monitoring glaucoma