Sensor fusion is most frequently discussed in smartphone and automotive control applications. However, the fusion aspect was initially created for military analysis. From the analysis standpoint, for improved decision-making, medical applications can and have benefited from sensor fusion. One example is in cancer detection and focused surgery. Specifically, the detection of and surgery for prostate cancer. According to the National Cancer Institute, prostate cancer is the most common cancer and the second leading cause of cancer death among men in the United States.
The prostate is a walnut-sized gland that is part of the male reproductive and urinary system. If a periodic blood test indicates increased or higher than normal prostate-specific antigen (PSA) levels, a doctor may recommend performing a magnetic resonance imaging (MRI) guided prostate biopsy.
MRI testing is used to analyze several potential problem areas in the human body including pancreas, kidneys, liver, bladder, and both male and female reproductive organs. For prostate cancer treatment, MRI-ultrasound fusion biopsy combines highly detailed MRI images with an ultrasound. Without involving radiation, MRI analysis uses magnets to collect detailed pictures of the prostate. The fusion or blending of sound waves in the ultrasound analysis provides more complete/detailed pictures to pinpoint any suspicious areas in the prostate.
The first step is an MRI. During the MRI, the patient may have a contrast dye injected through an intravenous (IV) needle to provide more detailed images. Prior to the use of MRI, a physician obtained 10 to 12 samples or cores as the first step using established transrectal ultrasound (TRUS) guidance. However, undersampling and overestimation of cancer were common.
As magnet quality increased from 0.3 tesla (T)–0.5 T to 1.5 T and even up to 3T, interest in MRI increased, and analysis improved as well. Further incremental gains occurred by using an endorectal coil (ERC) technique and multiphasic sequencing. With 3 T magnet devices, in addition to a stronger static magnetic field, the signal-to-noise ratio (SNR) is linearly higher than 1.5 T. While the ERC requirement is minimal, its use is still recommended. A newer MRI approach is called a multiparametric MRI (mpMRI). The highly sensitive mpMRI can identify cancerous areas better than a standard MRI.
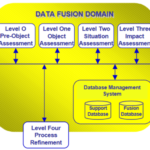
A highly experienced physician can combine mpMRI images with the real-time TRUS imaging technique (the cognitive fusion approach) and achieve acceptable results, but the use of software fusion for cancer detection makes all physicians operate at the highly experienced level or better. In either case, both are improvements over the standard TRUS-guided biopsy approach. This fused image helps the physician more precisely sample tissue from the identified problem areas. A mpMRI scan alone cannot diagnose prostate cancer, but it can help the doctor see:
- If there is an area in the prostate gland that looks suspicious
- If the patient needs a biopsy
- Specific location(s) to obtain the biopsies
- If the suspected cancer is confined to the prostate or has spread
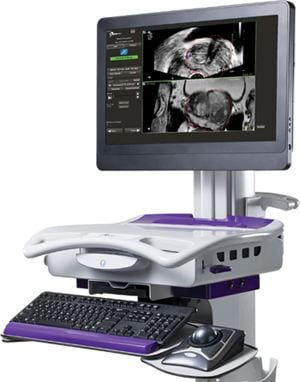 A fusion-guided prostate biopsy accomplishes three goals. First, it provides clear answers so doctors can tell the difference between aggressive prostate cancers and slow-growing ones. Secondly, it identifies aggressive tumors by enhancing the doctor’s ability to spot prostate tumors that need treatment. Finally, it helps prevent unnecessary procedures by avoiding treatment for slow-growing prostate tumors or repeat prostate biopsies. Within the last 10 years, the United States Food and Drug Administration (FDA) has approved at least four MRI/Ultrasound fusion biopsy devices.
A fusion-guided prostate biopsy accomplishes three goals. First, it provides clear answers so doctors can tell the difference between aggressive prostate cancers and slow-growing ones. Secondly, it identifies aggressive tumors by enhancing the doctor’s ability to spot prostate tumors that need treatment. Finally, it helps prevent unnecessary procedures by avoiding treatment for slow-growing prostate tumors or repeat prostate biopsies. Within the last 10 years, the United States Food and Drug Administration (FDA) has approved at least four MRI/Ultrasound fusion biopsy devices.
References
Image source: Multiparametric MRI (mpMRI) scan for prostate cancer
MRI-Ultrasound Prostate Fusion Biopsy
Image source: MRI/Ultrasound Fusion Biopsy
Prostate Cancer—Patient Version